The diagnosis of a terminal illness, particularly one with a prognosis of less than five years, casts a long shadow. It forces individuals to confront their mortality, grapple with end-of-life decisions, and often, explore all possible avenues for extending or improving their remaining time. In this context, the question arises: Should individuals facing a terminal diagnosis be permitted to utilize any treatment they deem helpful, regardless of its legality or the prevailing medical consensus? This paper argues that, while acknowledging the complexities and potential risks involved, individuals in such dire circumstances should be granted considerable autonomy in choosing their treatments, even if they fall outside conventional medical practice.
The Foundations of Autonomy and Self-Determination:
The ethical principle of autonomy dictates that individuals have the right to make informed decisions about their own bodies and healthcare. This principle is particularly potent when facing a terminal illness. With a limited lifespan, the perceived value of extending life, alleviating suffering, and maintaining dignity becomes paramount. Denying individuals access to treatments they believe might be beneficial infringes upon their autonomy and their right to self-determination. It implies a paternalistic approach, suggesting that medical professionals or the state know better than the individual experiencing the illness what is best for them.
The Limitations of Conventional Medicine and the Allure of Alternatives:
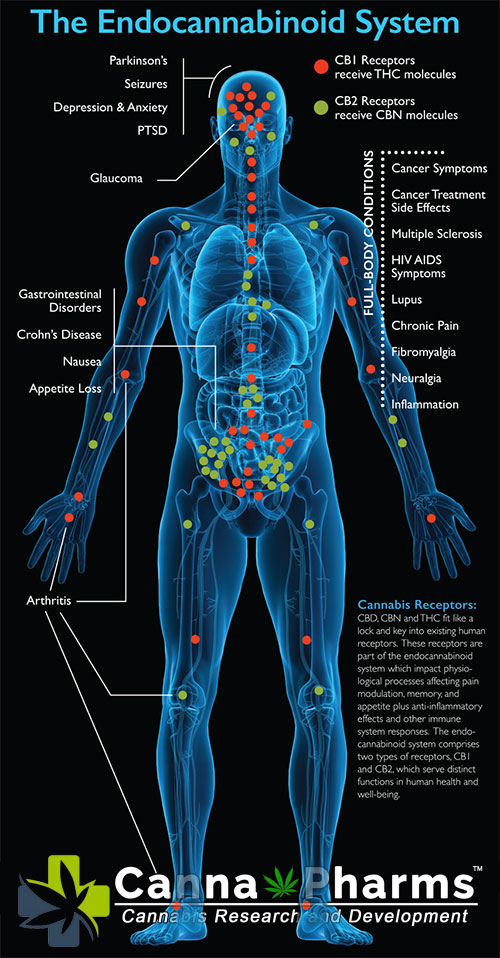
While conventional medicine offers remarkable advancements in treating and managing various diseases, it is not always successful in eradicating terminal illnesses. In some cases, treatments may be limited, offer only marginal improvements in quality of life, or carry debilitating side effects. This can lead individuals to seek alternative or complementary therapies, often driven by a desire for control, hope, and a personalized approach that resonates with their individual beliefs and experiences. These alternative treatments, even if lacking robust scientific validation, might offer psychological comfort, a sense of agency, or even, in rare cases, unexpected benefits.
The Spectrum of "Legal" and "Illegal" Treatments:
The legal status of a treatment is not always a reliable indicator of its efficacy or safety. Legal regulations are often influenced by political, economic, and social factors, and may not always reflect the latest scientific evidence. Moreover, treatments legal in one jurisdiction may be prohibited in another, creating a complex ethical landscape. "Illegal" treatments could encompass a range of options, from drugs unauthorized for a specific condition or dosage to therapies offered by unconventional practitioners. While due diligence is crucial, dismissing all illegal treatments outright based solely on their legal status is a rigid stance that fails to consider individual circumstances and potential benefits.
Navigating the Potential Risks and Harms:
Granting individuals access to unconventional treatments is not without its risks. These risks include:
- Financial Exploitation: Vunlerable individuals may be susceptible to fraudulent practitioners promising miracle cures.
- Physical Harm: Unproven treatments can have detrimental side effects and potentially hasten death.
- Delayed or Abandoned Conventional Care: Pursuing alternative therapies could distract from or replace evidence-based treatments that offer a greater chance of benefit.
- False Hope and Disappointment: The lack of scientific evidence supporting these treatments can lead to unrealistic expectations and ultimately, profound disappointment.
Mitigating Risks Through Informed Consent and Ethical Oversight:
To address these risks, several safeguards should be implemented:
- Informed Consent: Individuals must be provided with comprehensive information about the potential benefits, risks, and limitations of both conventional and unconventional treatments. They should be encouraged to discuss their choices with their physicians and family members.
- Transparency and Disclosure: Practitioners offering alternative treatments should be transparent about their qualifications, the evidence supporting their therapies, and any potential conflicts of interest.
- Independent Review Boards: Organizations could establish independent review boards to assess the ethical implications of unconventional treatments and provide guidance to individuals and their physicians. These boards could evaluate the scientific basis, potential risks, and ethical considerations of each treatment.
- Emphasis on Palliative Care: Regardless of treatment choices, access to comprehensive palliative care should be guaranteed to alleviate suffering, manage symptoms, and provide emotional support throughout the terminal illness journey.
The Argument for Compassionate Access and Experimental Treatments:
In situations where conventional treatments are exhausted, granting access to experimental or off-label treatments through compassionate access programs can be ethically justified. These programs allow individuals with life-threatening conditions to access investigational therapies that have not yet been fully approved by regulatory agencies. While such access should be carefully regulated and monitored, it offers a potential avenue for hope and improvement when all other options have been exhausted.
Conclusion:
The terminal diagnosis of an illness, especially with a limited prognosis, significantly alters the ethical considerations surrounding medical treatment. While acknowledging the potential risks inherent in unconventional and even illegal treatments, the principles of autonomy, self-determination, and compassion support granting individuals greater agency in choosing their own path. Implementing robust informed consent processes, promoting transparency, and establishing ethical oversight mechanisms are crucial to mitigating potential harms. Ultimately, the decision of how to spend one's remaining time in the face of a terminal illness should reside with the individual, empowering them to explore all reasonable options in their pursuit of hope, comfort, and a meaningful end-of-life experience. This approach necessitates a shift away from a purely paternalistic model of healthcare towards one that prioritizes patient autonomy and shared decision-making in the context of profound personal challenges.