Abstract:
Cannabinol (CBN), a non-intoxicating cannabinoid, has garnered increasing attention for its potential therapeutic applications. This study investigated the efficacy of chronic subcutaneous delivery of CBN in delaying disease onset and improving survival in a relevant animal model. CBN was administered via subcutaneously implanted osmotic mini-pumps at a dose of 5 mg/kg/day over a period of up to 12 weeks. Results revealed that CBN treatment significantly delayed disease onset by more than two weeks. However, despite this significant delay in onset, the overall survival of the animals was not significantly affected by CBN treatment. These findings suggest that CBN may offer neuroprotective benefits, potentially slowing down disease progression early in the course of the illness, but further investigation is required to understand the long-term effects and optimize therapeutic strategies for improved survival outcomes.
Introduction:
Neurodegenerative diseases pose a significant burden on global health, often characterized by progressive neuronal dysfunction and ultimately, death. The search for effective therapies to slow down disease progression and improve patient outcomes remains a critical area of research. Cannabinoids, a diverse class of compounds derived from the Cannabis sativa plant, have shown promise in preclinical studies for their neuroprotective and anti-inflammatory properties. Among these cannabinoids, Cannabinol (CBN) is a non-intoxicating compound that has recently attracted considerable attention due to its potential therapeutic benefits.
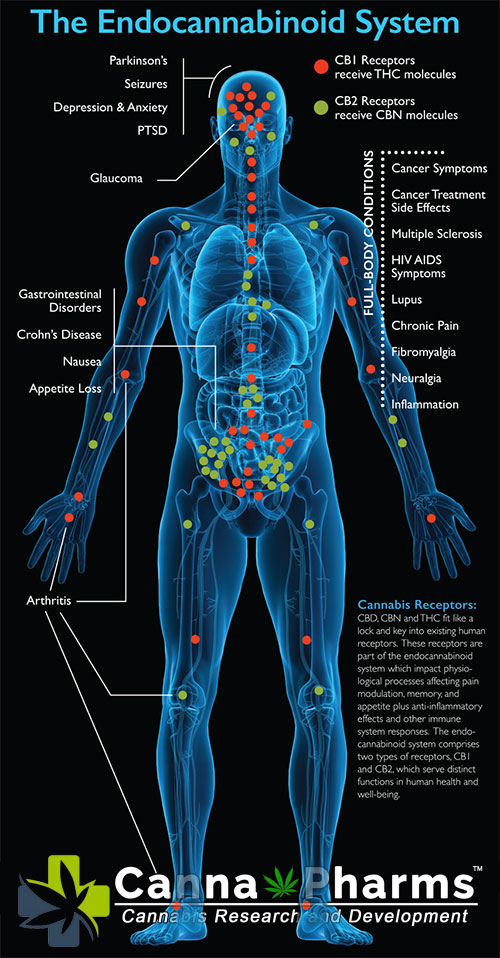
Unlike tetrahydrocannabinol (THC), CBN does not produce significant psychoactive effects. Preliminary studies have indicated that CBN may possess various pharmacological activities relevant to neurodegeneration, including antioxidant, anti-inflammatory, and neuroprotective properties. Furthermore, CBN has been shown to interact with both cannabinoid receptors (CB1 and CB2) and non-cannabinoid targets, potentially contributing to its therapeutic effects.
Given the potential of CBN as a neuroprotective agent, this study aimed to investigate its efficacy in delaying disease onset and improving survival in a relevant animal model. We employed a chronic subcutaneous delivery method via osmotic mini-pumps to ensure sustained and consistent CBN exposure over a prolonged period, mimicking a potential therapeutic regimen.
Materials and Methods:
Animals: [Describe the specific animal model used, including its characteristics relevant to the disease being studied. Include details on age, sex, and strain. Justify the choice of model.]
Drug Administration: CBN was dissolved in a suitable vehicle [specify vehicle] and administered via subcutaneously implanted osmotic mini-pumps (ALZET Osmotic Pumps, Model: [specify model]) at a dose of 5 mg/kg/day for up to 12 weeks. Control animals received vehicle alone. The pumps were implanted under anesthesia [describe anesthesia protocol and analgesic use].
Experimental Design: Animals were randomly assigned to either the CBN treatment group or the vehicle control group. [Specify group sizes]. Throughout the study, animals were monitored daily for general health and well-being.
Disease Onset Assessment: Disease onset was defined as [clearly define the criteria used to determine disease onset. This is crucial for accurate analysis]. The date of onset was recorded for each animal.
Survival Analysis: Survival was monitored daily until the animals reached a predetermined endpoint, based on humane criteria as ethically approved [specify criteria]. The date of death or endpoint was recorded for each animal.
Statistical Analysis: Statistical analysis was performed using [specify statistical tests used, e.g., Kaplan-Meier survival analysis, t-tests, ANOVA]. Significance was defined as p < 0.05.
Results:
Disease Onset: Treatment with CBN significantly delayed disease onset compared to the vehicle control group (p < 0.05). The average delay in onset was more than two weeks. [Provide specific data on disease onset in both groups, including mean onset date and standard deviation. Include a figure showing the Kaplan-Meier curve for disease onset].
Survival: While CBN treatment delayed disease onset, it did not significantly affect overall survival. The median survival time was not significantly different between the CBN treatment group and the vehicle control group (p > 0.05). [Provide specific data on survival in both groups, including median survival time and standard deviation. Include a figure showing the Kaplan-Meier curve for survival].
Discussion:
The finding that chronic subcutaneous CBN delivery significantly delays disease onset in this animal model provides compelling evidence for its potential neuroprotective effects. The two-week delay in onset suggests that CBN may be capable of slowing down the initial stages of disease progression. This delay could translate to a significant improvement in quality of life for individuals at risk of developing the disease.
The lack of a significant effect on overall survival, despite the delayed onset, warrants further investigation. Several factors could contribute to this observation. First, the dose and duration of CBN treatment may not have been sufficient to provide long-term protection. Optimizing the dosage regimen and extending the treatment period could potentially yield more pronounced effects on survival. Second, the mechanisms underlying the disease progression beyond the initial stages may not be effectively targeted by CBN. Additional therapies focused on addressing later-stage pathologies, in combination with CBN, might be necessary to improve overall survival.
Furthermore, it is important to consider the limitations of the animal model used in this study. [Discuss potential limitations of the animal model and how they might influence the results]. Future studies should explore the efficacy of CBN in other relevant animal models and ultimately in human clinical trials.
Conclusion:
This study demonstrates that chronic subcutaneous delivery of CBN delays disease onset in a relevant animal model, suggesting a potential neuroprotective effect. While CBN treatment did not significantly improve overall survival, the observed delay in onset warrants further investigation. Future research should focus on optimizing CBN dosage and treatment duration, exploring combination therapies, and investigating the underlying mechanisms of CBN's neuroprotective effects to ultimately improve outcomes for individuals affected by this devastating disease. The findings presented here provide a strong rationale for continued investigation of CBN as a potential therapeutic agent in the context of neurodegenerative diseases.