Abstract:
Amyotrophic Lateral Sclerosis (ALS), a devastating neurodegenerative disorder characterized by progressive motor neuron loss, remains a therapeutic challenge. While genetic and environmental factors are known contributors, emerging evidence highlights the critical role of the gut-brain axis in ALS pathogenesis. This paper explores the intricate connection between gut health, including gut microbiota composition and intestinal permeability, and ALS development and progression. We review the mechanisms through which gut dysbiosis can contribute to neuroinflammation, oxidative stress, and protein aggregation in the central nervous system, potentially influencing the onset and severity of ALS. Furthermore, we discuss potential therapeutic strategies targeting the gut microbiome, offering a promising avenue for mitigating disease progression and improving patient outcomes in ALS.
1. Introduction:
Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig's disease, is a fatal neurodegenerative disorder characterized by the progressive degeneration of motor neurons in the brain and spinal cord. This leads to muscle weakness, paralysis, and ultimately respiratory failure. While genetic mutations account for approximately 10% of ALS cases, the etiology of sporadic ALS remains largely unknown. Accumulating evidence suggests a complex interplay of genetic predisposition, environmental factors, and lifestyle influences contribute to disease onset and progression.
The gut-brain axis, a bidirectional communication network connecting the gastrointestinal tract and the brain, has garnered significant attention in recent years. This intricate system involves neural, hormonal, immune, and metabolic pathways. The gut microbiome, a complex community of microorganisms residing in the gut, plays a crucial role in regulating these pathways. Disruption of the gut microbiome, termed dysbiosis, can impact various aspects of health, including neurological function. Recent studies have implicated gut dysbiosis in the pathogenesis of several neurodegenerative diseases, including Parkinson's disease, Alzheimer's disease, and increasingly, ALS.
2. The Gut-Brain Axis: A Complex Communication Network:
The gut-brain axis facilitates bidirectional communication between the gut and the brain through several interconnected pathways:
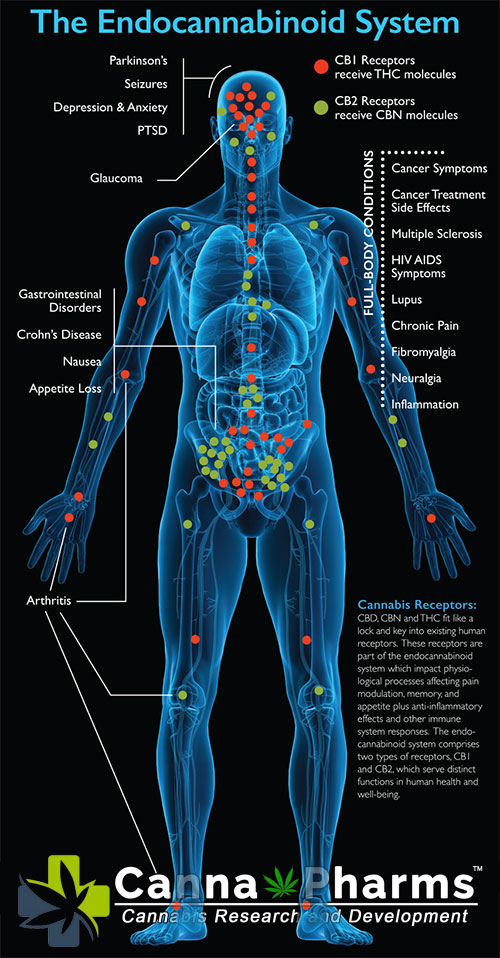
- Neural Pathways: The vagus nerve, a major component of the autonomic nervous system, directly connects the gut and the brain. Gut microbes can stimulate vagal afferent fibers, sending signals to the brainstem and influencing brain function.
- Hormonal Pathways: The gut produces a variety of hormones, such as serotonin and dopamine, which can directly impact brain function and mood. Changes in gut microbiome composition can alter the production of these hormones, potentially affecting neurological processes.
- Immune Pathways: The gut is a major immune organ, housing a large population of immune cells. Gut dysbiosis can trigger an inflammatory response in the gut, which can then spread systemically, leading to neuroinflammation.
- Metabolic Pathways: Gut microbes produce a variety of metabolites, such as short-chain fatty acids (SCFAs), which can cross the blood-brain barrier and influence brain function. SCFAs, in particular, have been shown to have neuroprotective effects.
3. Gut Dysbiosis in ALS: Evidence from Preclinical and Clinical Studies:
Mounting evidence suggests that gut dysbiosis is associated with ALS pathogenesis. Studies in animal models of ALS, particularly those using the SOD1-G93A transgenic mouse model, have demonstrated:
- Altered Gut Microbiome Composition: ALS mice exhibit significant alterations in gut microbial composition compared to control mice, with a reduction in beneficial bacteria, such as Butyricimonas, and an increase in potentially harmful bacteria, such as Ruminococcus and Escherichia. This dysbiosis typically precedes motor neuron degeneration.
- Increased Intestinal Permeability ("Leaky Gut"): ALS mice show increased intestinal permeability, allowing bacteria and their metabolites, such as lipopolysaccharide (LPS), to enter the bloodstream. This systemic inflammation can contribute to neuroinflammation.
- Exacerbated Disease Progression: Transferring gut microbiota from ALS mice to germ-free mice accelerated disease progression in these recipients, demonstrating a causal link between gut dysbiosis and ALS-like symptoms.
- Modulation of Gut Microbiota Improves Outcomes: Interventions aimed at modulating the gut microbiome, such as fecal microbiota transplantation (FMT) from healthy donors or the administration of specific probiotics, have shown promising results in ameliorating ALS-like symptoms in animal models.
Clinical studies in ALS patients have also reported significant differences in gut microbiome composition compared to healthy controls:
- Distinct Gut Microbiome Profiles: ALS patients exhibit a distinct gut microbiome profile characterized by decreased bacterial diversity and altered relative abundance of specific bacterial taxa. Some studies report a reduction in bacteria associated with SCFA production, potentially depriving the brain of neuroprotective metabolites.
- Correlation with Disease Severity: Certain gut microbiome signatures have been correlated with disease severity and progression rate in ALS patients. For example, an increase in Ruminococcus torques has been associated with faster disease progression.
- Increased Intestinal Permeability Evidence: Clinical studies have provided preliminary evidence of increased intestinal permeability in ALS patients, suggesting a potential link between gut leakiness and systemic inflammation.
4. Mechanisms Linking Gut Dysbiosis to ALS Pathogenesis:
Several mechanisms have been proposed to explain how gut dysbiosis can contribute to ALS pathogenesis:
- Neuroinflammation: Gut dysbiosis can trigger systemic inflammation, which can then lead to neuroinflammation. Pro-inflammatory cytokines, such as TNF-α and IL-1β, released from gut-associated immune cells can cross the blood-brain barrier and activate microglia, the resident immune cells of the brain. Activated microglia release further inflammatory mediators, contributing to neuronal damage and death.
- Oxidative Stress: Gut dysbiosis can lead to increased production of reactive oxygen species (ROS) in the gut and systemically. ROS induce oxidative stress, damaging cellular components, including proteins, lipids, and DNA. Oxidative stress is a well-established contributor to motor neuron degeneration in ALS.
- Protein Aggregation: Misfolded protein aggregation is a hallmark of ALS. Gut dysbiosis and the resulting inflammation and oxidative stress may contribute to protein misfolding and aggregation of proteins such as SOD1, TDP-43, and FUS, exacerbating neuronal dysfunction and cell death.
- Impaired SCFA Production: Decreased abundance of SCFA-producing bacteria can lead to reduced levels of SCFAs, which have neuroprotective effects. SCFAs can suppress inflammation, promote neuronal survival, and enhance blood-brain barrier integrity. Therefore, a deficiency in SCFAs may contribute to neurodegeneration in ALS.
- Altered Tryptophan Metabolism: Gut microbiota plays a crucial role in tryptophan metabolism, producing metabolites such as kynurenine and indole. Changes in gut microbiome composition can alter the balance of these metabolites, potentially impacting neuroinflammation and neuronal function.
5. Therapeutic Strategies Targeting the Gut Microbiome in ALS:
Given the growing evidence linking gut dysbiosis to ALS pathogenesis, targeting the gut microbiome represents a promising therapeutic avenue. Several strategies are being explored:
- Probiotics and Prebiotics: Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. Prebiotics are non-digestible food ingredients that promote the growth of beneficial gut bacteria. Clinical trials are investigating the potential of specific probiotics and prebiotics to improve gut health and mitigate ALS progression.
- Fecal Microbiota Transplantation (FMT): FMT involves transferring fecal matter from a healthy donor to the recipient to restore a healthy gut microbiome. While still in its early stages of development for ALS, FMT has shown promising results in animal models and warrants further investigation in clinical trials.
- Dietary Interventions: Diet plays a crucial role in shaping the gut microbiome. Specific dietary interventions, such as the ketogenic diet or a high-fiber diet, can alter gut microbiome composition and potentially influence disease progression.
- Antibiotics and Antimicrobials: While broad-spectrum antibiotics can have detrimental effects on the gut microbiome, selective antimicrobial agents targeting specific pathogenic bacteria may be beneficial in some cases. However, caution is warranted due to the potential for unintended consequences on the gut ecosystem.
6. Challenges and Future Directions:
Despite the promising results, several challenges remain in translating these findings into effective therapeutic strategies for ALS:
- Heterogeneity of the Gut Microbiome: Gut microbiome composition varies significantly between individuals due to genetic, environmental, and lifestyle factors. This heterogeneity makes it challenging to identify universal gut microbiome signatures associated with ALS and to develop personalized therapeutic interventions.
- Mechanism of Action: Further research is needed to fully elucidate the mechanisms by which gut dysbiosis contributes to ALS pathogenesis. Understanding these mechanisms will be crucial for developing targeted and effective therapies.
- Clinical Trial Design: Designing robust clinical trials to evaluate the efficacy of gut-targeted therapies in ALS is challenging. Factors such as patient heterogeneity, disease stage, and the complexity of the gut microbiome need to be carefully considered.
- Long-Term Effects: The long-term effects of gut-targeted therapies on ALS progression and patient outcomes need to be carefully evaluated.
Future research directions should focus on:
- Large-scale microbiome profiling studies: Conducting large-scale studies to identify specific gut microbiome signatures associated with ALS and to correlate these signatures with disease severity and progression.
- Mechanistic studies: Investigating the mechanisms by which specific gut microbes and their metabolites influence motor neuron function and survival.
- Personalized medicine approaches: Developing personalized therapeutic interventions based on individual gut microbiome profiles and disease stage.
- Combination therapies: Exploring the potential of combining gut-targeted therapies with other treatments, such as gene therapy or immunotherapy.
7. Conclusion:
The emerging evidence linking gut dysbiosis to ALS pathogenesis highlights the critical role of the gut-brain axis in disease development and progression. Gut dysbiosis can contribute to neuroinflammation, oxidative stress, and protein aggregation, potentially influencing the onset and severity of ALS. Targeting the gut microbiome represents a promising therapeutic avenue for mitigating disease progression and improving patient outcomes. Further research is needed to fully elucidate the mechanisms by which gut dysbiosis contributes to ALS and to develop personalized and effective gut-targeted therapies. By understanding and manipulating the complex interplay between the gut microbiome and the brain, we can potentially develop novel strategies to prevent, delay, or even reverse the devastating effects of ALS.